

Figure 1: Common clinical presentation of plantar plate injury with medial deviation of the toe and incisional placement.
Plantar plate pathology in conjunction with metatarsalgia occurs more often than is commonly appreciated, but can be addressed using a combined procedure that involves a dorsal approach to anatomic plantar plate repair and metatarsal realignment.
By Lowell Weil Jr, DPM, FACFAS, and Erin E. Klein, DPM, MS
French anatomist and pathologist Jean Cruveilhier first described the plantar plate in 1844. 1 Recently, this small structure has come to the forefront of forefoot reconstruction as a crucial part of the soft tissue balance of the lesser metatarsophalangeal (MTP) joints.
Metatarsalgia has been, and remains, one of the most common reasons that patients present to the foot and ankle specialist. One of the most common surgical techniques for treatment of this problem is a distal oblique shortening osteotomy 2 that was named the “Weil osteotomy” by orthopedic surgeon Louis Samuel Barouk, MD, of Bordeaux, France, after he visited Chicago foot and ankle surgeon Lowell Scott Weil Sr, DPM, many years ago.
All surgical procedures have problems and complications. The most commonly discussed problem associated with the Weil osteotomy is the floating toe, which in the literature has been reported to occur 15% to 50% of the time following a Weil osteotomy. 2-5 The floating toe is defined as a toe that does not touch the floor during neutral weight bearing after a metatarsal osteotomy. It is associated with weakness and decreased ability to actively plantar flex the toe.
Many authors have theorized about the cause of floating toe and have suggested modifications to the procedure to prevent its occurrence. However, most of these changes have not altered the outcome and have increased the incidence of other complications, including transfer metatarsalgia, stiffness, edema, and postoperative disability. 6-12
Proposed solutions have included making sure to perform the procedure starting in the articular surface to prevent plantar translation, appropriate dorsal soft tissue release, early physical therapy (seven days after surgery), and emphasizing plantar flexion strength and night splinting of the toe. Regardless, floating toes still occurred, and it was not unknown if the cause of this problem was related to osseous components of the lesser MTP joint, alteration of the joint axis, or the plantar soft tissues.

Figure 2: Cadaveric cross section with corresponding sagittal MRI demonstrating the plantar plate (pink arrows) and association with flexor tendons (yellow arrows).
There are few studies about the relevant surgical anatomy of the lesser MTP joint. Understanding this anatomy, however, is critical for understanding both the pathology and the surgical correction of this problem.
Advertisement
The plantar plate, situated on the plantar aspect of the metatarsal head, is 15 mm to 20 mm long, 16 mm wide, and 2 mm thick. 13,14 The proximal aspect of the plantar plate is the thinner more mobile attachment that attaches to the metatarsal proximal to the most proximal part of the articular cartilage. Distally, the plantar plate attaches to the base of the proximal phalanx in either one or two bands. The distal attachment of the plantar plate is stouter and less mobile than the proximal attachment. This is the portion of the plantar plate that is more often torn.
Laterally, the plantar plate is continuous with the deep transverse intermetatarsal ligament. It is this relationship that controls splay of the forefoot and keeps the digits in transverse plane rectus alignment. 15-18 The lateral portions of the plantar plate are also the sites of insertion of the accessory and suspensory collateral ligaments. 15,16 These ligaments originate from different portions of the tuberosity at the lateral metatarsal neck and are the anatomic landmarks for the blood vessels that supply blood to the metatarsal head and neck. 17
Plantar plate pathology seems to be more common than previously appreciated. As many as 50% of patients seen for metatarsalgia at our institution are patients seeking second opinions 19 and who had been seen by other physicians and treated for pathology (generally capsulitis or a second interspace neuroma) that was resistant to treatment. 19
Interestingly, in a cadaveric study 20 performed earlier this year that aimed at elucidating the cross-sectional anatomy of the metatarsal neck and the proximal attachment of the plantar plate, 80% (16 of 20) of these randomly selected specimens had one of four types 21 of plantar plate tears. 20
As with most pedal pathology, a thorough clinical exam is of paramount importance, as it is the first indicator that plantar plate pathology should be part of the differential diagnosis. In cases representing early stage disease, findings may be subtle.
Patients typically present with progressive pain to the ball of the foot that is localized to the plantar aspect of the MTP joint, the distal aspect of the metatarsal head, or both. 19,22 Numbness is occasionally present when edema presses on local nerves. 19 The toe (second, third, or both) may have slowly and progressively changed alignment to align more dorsally with either medial or lateral deviation (Figure 1). A modified drawer test may yield instability compared with the contralateral foot or compared to the “expected normal” result when bilateral pathology is present. 19,22,23

Figure 3: Proper positioning of McGlamry elevator to mobilize the plantar plate with preservation of collateral ligaments.
In the case of a partial or incomplete tear, the drawer test will often be painful. Hammertoe deformities may or may not be present. There may be plantar flexion weakness in the affected toe. There may or may not be concomitant first ray pathology (hallux valgus or hallux rigidus). 19,22
In end-stage disease (i.e., crossover toes and MTP joint dislocations), however, clinical findings may differ slightly. If the plantar plate is completely torn, pain and swelling in the area may be absent. 19,22 There may be a crossover toe or an MTP joint dislocation. 19,22 The drawer test may not be painful and may not be positive, particularly if the MTP joint is already dislocated. 22
Bilateral weight-bearing radiographs will often show an altered metatarsal pattern, including a second metatarsal that is subtly longer compared with the contralateral foot, 24 transverse plane deviation of the digits, 3,24 splaying of the digits, and a subtly increased metatarsus adductus angle. 24 Interestingly, 60% of our plantar plate pathology patients with splaying of the second and third digits did not have an interdigital neuroma. 3,19,24
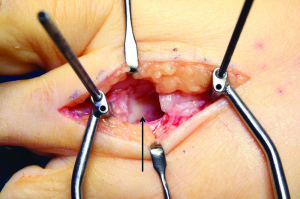
Figure 4: Visualization of the plantar plate (black arrow) from the dorsal approach with distraction device in place.
The sensitivity and specificity of clinical 19 and radiographic 24 exam parameters, when compared with intraoperative pathology, have been published previously. When analyzed individually there are many exam parameters that appear to be both sensitive and specific for this pathology. However, the astute physician does not typically rely on a single parameter for diagnosis. For this reason, the clinical and radiographic exam parameters studied previously were entered into a logistic regression model to determine which parameter or combination of parameters were most important in differentiating high-grade plantar plate tears from low-grade tears. 25
We found a positive drawer sign was the most informative individual test for differentiating high- and low-grade plantar plate tears (sensitivity 91.5%, specificity 22%). 25 Most radiographic parameters did little to aid in the diagnosis as this is primarily a soft tissue pathology. However, adding the third MTP joint transverse deviation angle (> 15º) to the model best improved the accuracy of a good clinical exam. 25 When a positive drawer sign was combined with symptoms present for more than two years and an MTP joint deviation angle greater than 15º in either direction, we obtained the greatest specificity (89.1%) of any combination of parameters. 25 This study of clinical and radiographic parameters found lower sensitivities and specificities than expected, highlighting the need for understanding and accuracy in advanced diagnostic imaging.

Figure 5: Plantar plate (black arrow) completely detached from proximal phalanx with flexor tendons in close plantar proximity (green arrow). Note the thickness of the plantar plate.
In the past, advanced diagnostics were inconsistent at best. Magnetic resonance imaging (MRI) of an MTP joint would rarely provide more than one or two slices through the joint. Between the thickness of the slices and the volume-averaging techniques used in MRIs, visualization of the plantar plate was poor and thoroughly inadequate. More current MRI techniques allow much better visualization of the MTP joint (Figure 2).
Sung et al 26 conducted a study to determine MRI correlation to intraoperative findings of plantar plate pathology without intravenous contrast and without intra-articular contrast, as had been done previously in the literature. 13,14,27,28 In this study the overall accuracy of MRI for detecting plantar plate pathology was 96%. The study found a sensitivity of 95%, a specificity of 100%, a positive predictive value of 100%, and a negative predictive value of 67%.
Researchers have also investigated diagnostic ultrasound for preoperative evaluation of plantar plate pathology. 13,29 In a study of 50 consecutive patients with forefoot pain and a suspected unilateral plantar plate tear at the second MTP joint 29 longitudinal ultrasound images correctly identified 40 of 45 plantar plate tears that were confirmed intraoperatively. The longitudinal ultrasound had a sensitivity of 91.1%, a specificity of 25%, a positive predictive value of 91.1%, and a negative predictive value of 25%. Transverse ultrasound images identified 36 plantar plate tears, correctly localizing only 19 tears.
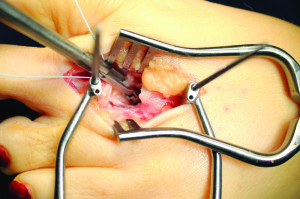
Figure 6: Mini Scorpion (Arthrex) grasping plantar plate and engaging suture.
One of the cited benefits of ultrasound is the ability to do a dynamic examination. 13,27 An ongoing study at our institution 30 has investigated this concept in 36 consecutive patients with second MTP joint pain. In the 45 MTP joints included, we identified 38 plantar plate tears intraoperatively. Static examination 30 of these joints had a sensitivity and specificity of 81.6% and 71.4%, respectively. The dynamic examination 30 had a sensitivity of 100% and a specificity of 85.7%. In both of these studies the ability of the ultrasound to detect the presence or absence of plantar plate pathology was high, but its ability to accurately detect the location of pathology was low. 30
To our knowledge, only two studies in the literature have directly compared ultrasound and MRI imaging of the plantar plate. 27,31 One looked only at cadaveric specimens 27 while the other compared preoperative MRI and ultrasound with intraoperatively identified pathology. 31
The cadaveric study 27 found ultrasound was more sensitive and accurate than MRI for identifying plantar plate pathology. In the second study 31 researchers conducted a head-to-head comparison of ultrasound and MRI to intraoperative findings in 42 consecutive patients with suspected plantar plate pathology. Physicians conducted preoperative MRI and ultrasound and, when reading images, were blinded to findings from patients’ clinical and radiographic exams, as well as each other’s exam findings. All patients were examined in the operating room, and 46 plantar plate tears were identified.
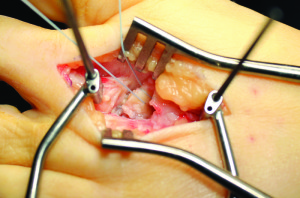
Figure 7: Plantar plate with mattress suture in place.
The sensitivity, specificity, positive predictive value, and negative value of MRI were 73.9%, 100%, 100%, and 29.4%, respectively; the same values for ultrasound were 91.5%, 25%, 91.5%, and 25%, respectively. MRI identified four collateral ligament tears not identified on ultrasound. The researchers concluded that both MRI and ultrasound are appropriate modalities for imaging of the plantar plate. While ultrasound is a highly sensitive exam, MRI is a more specific exam. In addition, MRI has the potential to be a much more standardized exam, while ultrasound has the potential for more variation. Overall, these results do not suggest ultrasound should replace MRI in all cases.
Previously, for cases in which plantar plate pathology and metatarsal deformity were present, surgeons would have to choose whether to realign the metatarsal or repair the plantar plate. Plantar plate repair was typically approached from the plantar surface of the foot, which violated important anatomy, may not have provided adequate visualization of the relevant pathology, and had the potential to leave a painful scar. To address these challenges, we have developed a combined procedure that involves a dorsal approach to anatomic plantar plate repair and Weil osteotomy. 32
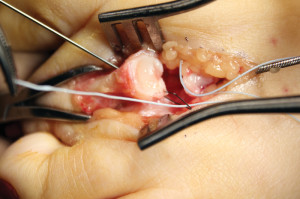
Figure 8: Oblique bone tunnel with suture passer in place to pass suture securing plantar plate into proximal phalanx.
A linear incision overlying the extensor apparatus is made extending from the distal third of the metatarsal shaft to the midshaft of the proximal phalanx, centering over the MTP joint (Figure 1). After dissection down to the extensor apparatus, an incision to the level of bone is created between the extensor digitorum longus and the extensor digitorum brevis, running from the distal metatarsal to the proximal phalanx shaft. A self-retainer is placed deep to the extensor tendons and the MTP joint is exposed. The medial and lateral collateral ligaments are reflected off the proximal phalanx base, and care should be taken so that the metatarsal head attachments are preserved.
A small or medium metatarsal elevator is then carefully placed into the MTP joint and advanced proximally (hugging the bone) to release adhesions and mobilize the proximal plantar plate attachment at the metatarsal neck, allowing improved exposure to the plantar plate later in the procedure. The elevator should only be used plantarly and not carried to the medial or lateral side of the metatarsal head. The collateral attachments, which are the most important means of blood supply to the metatarsal head, 33 must be maintained (Figure 3).
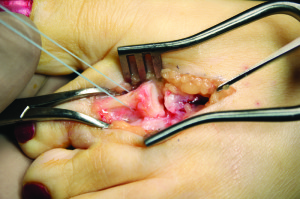
Figure 9: Sutures securely in place through bone tunnels pulling plantar plate into proximal phalanx.
A Weil osteotomy is performed in the metatarsal. 2 The osteotomy starts in the dorsal (2-3 mm) articular surface of the metatarsal. The angle of the osteotomy should be as close as possible to parallel to the weight-bearing surface. This angle is important to prevent plantar displacement of the metatarsal head as shortening is created.
Once the osteotomy is complete, a metatarsal pushing device is used to push the metatarsal head proximally 7 to 15 mm, where it is temporarily fixated with a 1.6-mm threaded Kirschner wire or pin.
A mini-joint distraction device is placed over the pin, fixating the metatarsal head, and a second pin is inserted from dorsal to plantar, 5 mm distal to the base of the proximal phalanx. The distractor is then opened, allowing dorsal access to the MTP joint and visualization of the plantar plate (Figure 4).
Plantar plate pathology can be confirmed with direct visualization of this structure. We have observed several different types of plantar plate injuries: 21 attenuation and attrition, longitudinal buttonhole tears, partial transverse tears, and complete ruptures (Table 1). The most common pattern, both in cadavers and our patients, is incomplete transverse tears at the site of attachment to the proximal phalanx. These tears can be seen at the medial or, more commonly, the lateral plantar plate attachment. In more advanced disease, the entire plantar plate will be torn. Nery et al 21 published an anatomic study in 2012 that both identified and classified plantar plate tears. This system is the most widely used classification system for this problem. 21

If the plantar plate has pathology, its entirety must be carefully dissected off the base of the proximal phalanx (Figure 5). The flexor tendons run in close plantar (deep) proximity to the plantar plate at this level, and care must be taken not to transect them. Once the plantar plate has been resected off the phalanx, dissection should be done proximally to create a full thickness flap of plantar plate for advancement. A freer elevator may be helpful to maintain a consistent level of tissue during this dissection.
Once the plantar plate has been completely mobilized, a miniature suturing device is used to create a wide three-stitch mattress (Figures 6 and 7). The distraction device is removed, a right angle towel clamp is placed around the sides of the proximal phalanx, and manual distraction/plantar flexion is performed to expose the base of the proximal phalanx. Any soft tissue attachments on the plantar surface of the proximal phalanx base are removed. The plantar bony surface is roughened with a small curette to facilitate plantar plate reattachment.
Crossed bone tunnels are created in the proximal phalanx, from distal dorsal medial to proximal plantar lateral (Figure 8). A second tunnel is created by drilling from distal dorsal lateral to proximal plantar medial. The sutures attached to the plantar plate are then passed from plantar to dorsal through the bone tunnels in the phalanx (Figure 9).
The temporary fixation for the metatarsal head is now removed and the metatarsal head is pulled to the desired length. It is rare for shortening to exceed 3 mm. Once accurate alignment is achieved, the osteotomy is fixated with one or two snap-off screws.

Figure 10: Proper position of the toe after osteotomy fixated and sutures secured dorsally.
The phalanx is plantar flexed to approximately 15°-20°. The sutures are then pulled tightly to advance the plantar plate into the base of the proximal phalanx. The sutures are tied dorsally to secure the plantar plate position. The toe will appear plantar flexed (Figure 10). Deep tissue and skin are then reapproximated and a bulky compressive bandage applied to hold the second toe in plantar flexion. This bandage should remain in place for seven to 10 days, with the patient allowed guarded partial weight bearing in a surgical shoe.
Bandages are removed seven to 10 days postoperatively, and the patient is instructed to return to a supportive athletic shoe with guarded weight bearing. The patient is also dispensed a night brace to reduce swelling and serve as a night splint to hold the toe in plantar flexion (Figure 11). This night splinting technique helps prevent dorsal contracture and scar tissue formation that can lead to limited postoperative plantar flexion.
Aggressive physical therapy is also started at seven to 10 days postoperative with particular emphasis on plantar flexion and intrinsic muscle strength. Passive and active range of motion of the short and long flexor tendons, often under the direction of a physical therapist two to three times per week, is often included in the postoperative regimen.
Patients are able to return to normal shoe gear and begin aggressive weight-bearing activities six to eight weeks postoperatively.

Figure 11: Bioskin AFTR DC postoperative brace with osteotomy strap holding toe in plantar flexed position.
We published early results of this procedure in 13 patients (15 feet) in 2011. 32 Pain decreased from 7.3 out of 10 + 1.6 preoperatively to 1.7 out of 10 + 1.8 postoperatively on the visual analog scale (p < .0001). Eighty five percent of patients reported improved function and 77% were satisfied or very satisfied with the outcome.
Two complications occurred in this group of patients: painful hardware and continued metatarsalgia. There were no incidences of dehiscence, malunion, nonunion, or recurrent MTP joint subluxation or dislocation.
Since the time of that study’s publication, we have performed approximately two hundred of these procedures, all with similar and significant postoperative reduction in pain level. A few patients have sustained significant painful stiffness postoperatively that has resolved after a joint manipulation under anesthesia. We plan to publish results of longer follow up in this larger cohort of patients in the next 12 months or so.
Metatarsalgia is one of the most common problems presenting to foot and ankle specialists. Typically, the position and length of the second metatarsal (and occasionally the third) has created a biomechanical imbalance in the forefoot, causing pain and subsequent injury to the surrounding soft tissue structures, particularly the plantar plate. 24
During the propulsive phase of gait, a metatarsal that is elongated will be overloaded with every step. Over time, that overload will cause attrition to the plantar plate and imbalance in the surrounding soft tissue structures, leading to pain, swelling, and deviation of the joint. The extensor tendons, which already have a mechanical advantage at the lesser MTP joint, will be able to exert more of a deforming force at this joint. The flexor tendons will lose the ability to plantar flex the proximal phalanx, since an intact and functioning plantar plate is required for plantar flexion. The more the MTP joint is deviated, particularly in the sagittal plane, the more this muscle imbalance is accentuated.
Radiographically, patients with plantar plate pathology tend to have a subtle difference in the length of the second metatarsal compared with the contralateral foot (for unilateral pathology) or when compared with the expected normal second metatarsal protrusion distance (for bilateral pathology). 22,24 In our patients with unilateral plantar plate tears, the side with the plantar plate pathology had a second metatarsal protrusion distance of 4.4 + 1 mm, which is .6 mm longer than the contralateral/nonpathological side (3.8 + 1 mm). 24
Taking these two things together, it seems that plantar plate pathology is accompanied by an underlying osseous deformity. 24 This is similar to the concept of lateral ankle instability with a subtle cavus deformity 34-38 or a posterior tibial tendon dysfunction with a valgus deformity of the calcaneus. 39-42 In both cases, the literature 34-42 supports correcting the osseous deformity and the soft tissue problem, as doing either procedure alone leads to suboptimal results. Why would the forefoot be any different?
Without metatarsal shortening, soft tissue corrections will fail over time, just as repairing a posterior tibial tendon without changing the structure of the rearfoot will fail over time.
The plantar plate is one of the main stabilizers of the lesser metatarsophalangeal joint. 15,17,18,22,23,43 In concert with the collateral ligament complex, 16 sagittal and transverse plane deformity (including dislocation) are resisted at the level of the MTP joint.
Sectioning of the plantar plate will decrease the amount of force necessary to dislocate the MTP joint by 30%. 44 Sectioning of the collateral ligaments will decrease the amount of force to dislocate the MTP joint by 45%. 44 Sectioning both structures will decrease the amount of force needed to dislocate the MTP joint by 79%. 44
It stands to reason, therefore, that pathology of the plantar plate needs to be repaired to restore stability to the lesser MTP joint. This concept is similar to that of a Brostrom procedure for lateral ankle stabilization: when the primary stabilizing structure of a joint is repaired, the joint becomes more stable.
The incidence of plantar plate pathology is far higher than is commonly appreciated by most physicians. In previous cadaveric dissection with random selection of cadaveric specimens, 80% (16 of 20) had plantar plate pathology. 20 This suggests the incidence of plantar plate tears in the living population also may be higher than previously appreciated.
The clinical application of this concept 19 involves adding plantar plate pathology to the differential diagnosis of metatarsalgia and forefoot pain. An appropriate clinical exam, particularly in patients with a positive drawer sign and a transverse plane deviation of more than 15º in the third digit on weight-bearing radiographs, should point the astute clinician toward the diagnosis of a plantar plate problem. 19,24,25 Although both ultrasound and MRI can detect plantar plate pathology, 31 MRI may be the better exam as the protocol can be standardized. 31 As noted, ultrasound exam findings may vary based on technician experience and technique. 29-31
The dorsal approach to plantar plate repair provides a combined alternative to fully correct the complex nature of both a plantar plate tear and a metatarsal deformity. 32 The dorsal approach of this procedure allows the surgeon to appreciate both subtle and more severe plantar plate injuries that may not be clearly evident when using a plantar approach, while allowing for metatarsal realignment and preventing a plantar scar. With further attention and research, plantar plate problems will be better understood, diagnosed, and treated to provide patients and surgeons with optimal results.
Lowell Weil Jr, DPM, FACFAS, is president and fellowship director of the Weil Foot & Ankle Institute, which has 11 locations in the Chicago area. He also serves as editor of Foot and Ankle Specialist. Erin E. Klein, DPM, MS, is an associate at the Weil Foot & Ankle Institute and a clinical instructor in the Department of Applied Biomechanics and Surgery at the Dr. William M. Scholl College of Podiatric Medicine in North Chicago.
REFERENCES1. Cruveilhier J. The Anatomy of the Human Body. New York: Harper and Brother’s; 1844.
2. Barouk LS. Weil’s metatarsal osteotomy in the treatment of metatarsalgia. Orthopade 1996;25(4):338-344.
3. Coughlin MJ. Subluxation and dislocation of the second metatarsophalangeal joint. Orthop Clin North Am 1989;20(4):535-551.
4. Coughlin MJ. Crossover second toe deformity. Foot Ankle 1987;8(1):29-39.
5. Migues A, Slullitel G, Bilbao F, et al. Floating-toe deformity as a complication of the Weil osteotomy. Foot Ankle Int 2004;25(9):609-613.
6. Coughlin MJ, Schutt SA, Hirose CB, et al. Metatarsophalangeal joint pathology in crossover second toe deformity: a cadaveric study. Foot Ankle Int 2012;33(2):133-140.
7. Highlander P, VonHerbulis E, Gonzalez A, et al. Complications of the Weil osteotomy. Foot Ankle Spec 2011;4(3):165-170.
8. Garg R, Thordarson DB, Schrumpf M, Castaneda D. Sliding oblique versus segmental resection osteotomies for lesser metatarsophalangeal joint pathology. Foot Ankle Int 2008;29(10):1009-1014.
9. Joseph R, Schroeder K, Greenberg M. A retrospective analysis of lesser metatarsophalangeal joint fusion as a treatment option for hammertoe pathology associated with metatarsophalangeal joint instability. J Foot Ankle Surg 2012;51(1):57-62.
10. Baravarian B, Thompson J, Nazarian D. Plantar plate tears: a review of the modified flexor tendon transfer repair for stabilization. Clin Podiatr Med Surg 2011;28(1):57-68.
11. Bouché RT, Heit EJ. Combined plantar plate and hammertoe repair with flexor digitorum longus tendon transfer for chronic, severe sagittal plane instability of the lesser metatarsophalangeal joints: preliminary observations. J Foot Ankle Surg 2008;47(2):125-137.
12. Klammer G, Baumann G, Moor BK, et al. Early complications and recurrence rates after Kirschner wire transfixion in lesser toe surgery: a prospective randomized study. Foot Ankle Int 2012;33(2):105-112.
13. Gregg JM, Silberstein M, Schneider T, et al. Sonography of plantar plates in cadavers: correlation with MRI and histology. AJR Am J Roentgenol 2006;186(4):948-955.
14. Gregg J, Marks P, Silberstein M, et al. Histologic anatomy of the lesser metatarsophalangeal joint plantar plate. Surg Radiol Anat 2007;29(2):141-147.
15. Deland JT, Lee KT, Sobel M, DiCarlo EF. Anatomy of the plantar plate and its attachments in the lesser metatarsal phalangeal joint. Foot Ankle Int 1995;16(8):480-486.
16. Deland JT, Sung IH. The medial crosssover toe: a cadaveric dissection. Foot Ankle Int 2000;21(5):375-378.
17. Johnston RB 3rd, Smith J, Daniels T. The plantar plate of the lesser toes: an anatomical study in human cadavers. Foot Ankle Int 1994;15(5):276-282.
18. Stainsby GD. Pathological anatomy and dynamic effect of the displaced plantar plate and the importance of the integrity of the plantar plate-deep transverse metatarsal ligament tie-bar. Ann R Coll Surg Engl 1997;79(1):58-68.
19. Klein EE, Weil L Jr, Weil LSS, et al. Clinical examination of plantar plate abnormality: a diagnostic perspective. Foot Ankle Int 2013;34(6):800-804.
20. Klein EE, Weil L Jr, Weil LSS, Bareither D. Incidence of plantar plate tears and associated anatomic variations of the second metatarsophalangeal joint. In press.
21. Nery C, Coughlin MJ, Baumfeld D, Mann TS. Lesser metatarsophalangeal joint instability: prospective evaluation and repair of plantar plate and capsular insufficiency. Foot Ankle Int 2012;33(4):301-311.
22. Kaz AJ, Coughlin MJ. Crossover second toe: demographics, etiology, and radiographic assessment. Foot Ankle Int 2007;28(12):1223-1237.
23. Thompson FM, Hamilton WG. Problems of the second metatarsophalangeal joint. Orthopedics 1987;10(1):83-89.
24. Klein EE, Weil L Jr, Weil LSS, Knight J. The underlying osseous deformity in plantar plate tears: a radiographic analysis. Foot Ankle Spec 2013;6(2):108-118.
25. Weil L Jr, Weil LS Sr, Fleischer AE, Bowen MF. Positive drawer test combined with radiographic transverse plane deformity of the 3rd metatarsophalangeal joint suggests high grade tears of the 2nd metatarsophalangeal joint plantar plate. In press.
26. Sung W, Weil L Jr, Weil LSS, Rolfes RJ. Diagnosis of plantar plate injury by magnetic resonance imaging with reference to intraoperative findings. J Foot Ankle Surg 2012;51(5):570-574.
27. Gregg J, Silberstein M, Schneider T, Marks P. Sonographic and MRI evaluation of the plantar plate: A prospective study. Eur Radiol 2006;16(12):2661-2669.
28. Kier R, Abrahamian H, Caminear D, et al. MR arthrography of the second and third metatarsophalangeal joints for the detection of tears of the plantar plate and joint capsule. AJR Am J Roentgenol 2010;194(4):1079-1081.
29. Klein EE, Weil L Jr, Weil LSS, Knight J. Musculoskeletal ultrasound for preoperative imaging of the plantar plate: a prospective analysis. Foot Ankle Spec 2013;6(3):196-200.
30. Feuerstein CA, Weil L Jr, Weil LS Sr, Klein EE. Static and dynamic musculoskeletal ultrasound for detection of plantar plate pathology. In press.
31. Klein EE, Weil L Jr, Weil LSS, Knight J. Magnetic resonance imaging versus musculoskeletal ultrasound for identification and localization of plantar plate tears. Foot Ankle Spec 2012;5(6):359-365.
32. Weil L Jr, Sung W, Weil LSS, Malinoski K. Anatomic plantar plate repair using the Weil metatarsal osteotomy approach. Foot Ankle Spec 2011;4(3):145-150.
33. Petersen WJ, Lankes JM, Paulsen F, Hassenpflug J. The arterial supply of the lesser metatarsal heads: a vascular injection study in human cadavers. Foot Ankle Int 2002;23(6):491-495.
34. Irwin TA, Anderson RB, Davis WH, Cohen BE. Effect of ankle arthritis on clinical outcome of lateral ankle ligament reconstruction in cavovarus feet. Foot Ankle Int 2010;31(11):941-948.
35. Morrison KE, Kaminski TW. Foot characteristics in association with inversion ankle injury. J Athl Train 2007;42(1):135-142.
36. Vienne P, Schöniger R, Helmy N, Espinosa N. Hindfoot instability in cavovarus deformity: static and dynamic balancing. Foot Ankle Int 2007;28(1):96-102.
37. Sammarco GJ, Taylor R. Cavovarus foot treated with combined calcaneus and metatarsal osteotomies. Foot Ankle Int 2001;22(1):19-30.
38. Larsen E, Angermann P. Association of ankle instability and foot deformity. Acta Orthop Scand 1990;61(2):136-139.
39. Chan JY, Williams BR, Nair P, et al. The contribution of medializing calcaneal osteotomy on hindfoot alignment in the reconstruction of the stage II adult acquired flatfoot deformity. Foot Ankle Int 2013;34(2):159-166.
40. Kou JX, Balasubramaniam M, Kippe M, Fortin PT. Functional results of posterior tibial tendon reconstruction, calcaneal osteotomy, and gastrocnemius recession. Foot Ankle Int 2012;33(7):602-611.
41. Smith JT, Bluman EM. Update on stage IV acquired adult flatfoot disorder: when the deltoid ligament becomes dysfunctional. Foot Ankle Clin 2012;17(2):351-360.
42. Oh I, Williams BR, Ellis SJ, e al. Reconstruction of the symptomatic idiopathic flatfoot in adolescents and young adults. Foot Ankle Int 2011;32(3):225-232.
43. Coughlin MJ. Second metatarsophalangeal joint instability in the athlete. Foot Ankle 1993;14(6):309-319.
44. Bhatia D, Myerson MS, Curtis MJ, et al. Anatomical restraints to dislocation of the second metatarsophalangeal joint and assessment of a repair technique. J Bone Joint Surg Am 1994;76(9):1371-1375.